What To Do About America's Shrinking Life Expectancy? | Opinion
The land of the free is experiencing a disturbing trend: Americans are dying younger. While boasting some of the highest health care expenditures in the world, the most advanced medical technologies, and recent expansion of government-sponsored health care coverage, this begs the question—what is American health care getting wrong?
But that question is itself part of the problem. We've assigned life expectancy to the domain of health care when the true issues stem from deep political and societal quagmires stuck in partisan stalemates as our years of life continue to ebb away.
No discussion of American health is complete without addressing obesity. As doctors wag their fingers at patients, touting healthy foods, and the American Heart Association's guidelines for 150 minutes of exercise per week pale in comparison to the magnitude of the social predicaments that led us to this point.
An estimated 54 million Americans live in food scarcity, and no amount of nutrition counseling can mitigate the reality of food deserts. Americans also have some of the highest work hours in the world, making those 150 minutes of exercise difficult to fit into crammed schedules. Access to parks is disparate across the nation, predictably worse in impoverished areas, where outdoor activity is most needed to combat obesity.
Health care has taken on the helm of educating about the dangers of obesity. We certainly need it given that we have the highest chronic disease burden of any industrialized country, but the issue now is not that our words are falling on deaf ears, they're falling on resource-starved communities. And that's an issue health care can't solve.
Competing political forces further exacerbated the state of obesity in our country. Following the money reveals a disheartening narrative of politics and special interests, sacrificing our health for dollars. "Big Food" championed the fast food industry, processed foods, and saturated fats, while "Big Alcohol" pushed marketing and PAC dollars to Congress. All the while, health care reimbursement for obesity and nutrition counseling remained grossly inadequate. In the fight against the 800-pound gorilla of the obesity epidemic in America, we've got nothing but empty words.
This paradigm extends beyond just obesity.
The opioid crisis, another major contributor to lower life expectancy, is just as problematic. Born from unrestrained Big Pharma, this epidemic in America has been met with unrelenting hurdles rooted in politics. Naloxone, a opioid reversal agent that is life-saving in the cases of opioid overdoses, is finally available over the counter in all states, but still remains prohibitively expensive for many Americans. It wasn't until this year that buprenorphine, a drug used for long-term medication assisted therapy for opioid use disorder, was available to be prescribed by doctors without a cumbersome-to-obtain license called the X Waiver. Nonetheless, there still remain major challenges to patient access to buprenorphine tied to lack of billing and reimbursement, burdensome prior authorization requirements, and lack of outpatient resources. Frustratingly, in this instance, we have the tools to help, but our tools are constrained by administrative red tape.

Both buprenorphine and naloxone mitigate the rate of opioid deaths, but don't address the root cause of addiction. To tackle this, we must confront the overarching issue of mental health. Our health care system is undoubtedly underfunded and under resourced to meet our nation's behavioral health needs. Our suicide rates are some of the highest among industrialized countries. We must grapple with the reasons behind our immense mental health burden, and more importantly, determine how to alleviate it.
Sure, we have Zoloft and Prozac, but they don't resolve societal stressors like high divorce rates, the negative impact of social media, or a dearth of early childhood systems that can foster emotional and mental resilience from a young age. By the time a patient sees me in the emergency department in acute suicidal crises, it is already too late.
The physical health of our children is also hanging in the balance. A staggering 20 percent of children in the United States live in relative poverty, compared to a 13 percent average across OECD countries. The ramifications for health are clear—higher obesity rates, increased chronic health burden, heightened risk of violence. While we can't eliminate economic disparities, we can strive to provide support—yet even our support is woefully under-funded. Medicaid provides health care coverage for roughly half of children in the United States, yet its reimbursement rates are 72 cents on the dollar. If we truly believe in investing in our future, we must put our money where our hearts are.
As an ER doctor, I thought I was entering a profession to battle disease and fight illness. Instead, I find myself continually challenged by the Goliaths of social, economic, and political forces, armed with not even a slingshot.
Our arsenal of interventions easily encompasses medicines, surgeries, diagnostics, and minimally invasive procedures. However, these instruments aren't effective in addressing any of the underlying reasons for our poor health status.
To truly improve the health of America, we must look beyond the medical realm and push for comprehensive, systemic change. The root causes lie with social determinants of health, and the solutions lie with our legislators. We need solutions to improve food resources, community safety, and neighborhood environments. We need a public health care system that prioritizes the needs of our most vulnerable populations. We need safeguards against profit-driven motives of private corporations and special interest groups.
The decline in America's health, as evidenced by shrinking life expectancy and the limitations of health care, demands a collective response.
In order to foster a healthier America, we must acknowledge that the responsibility extends beyond health care providers alone. We want to be part of the solution, but we can't be the sole lifeline.
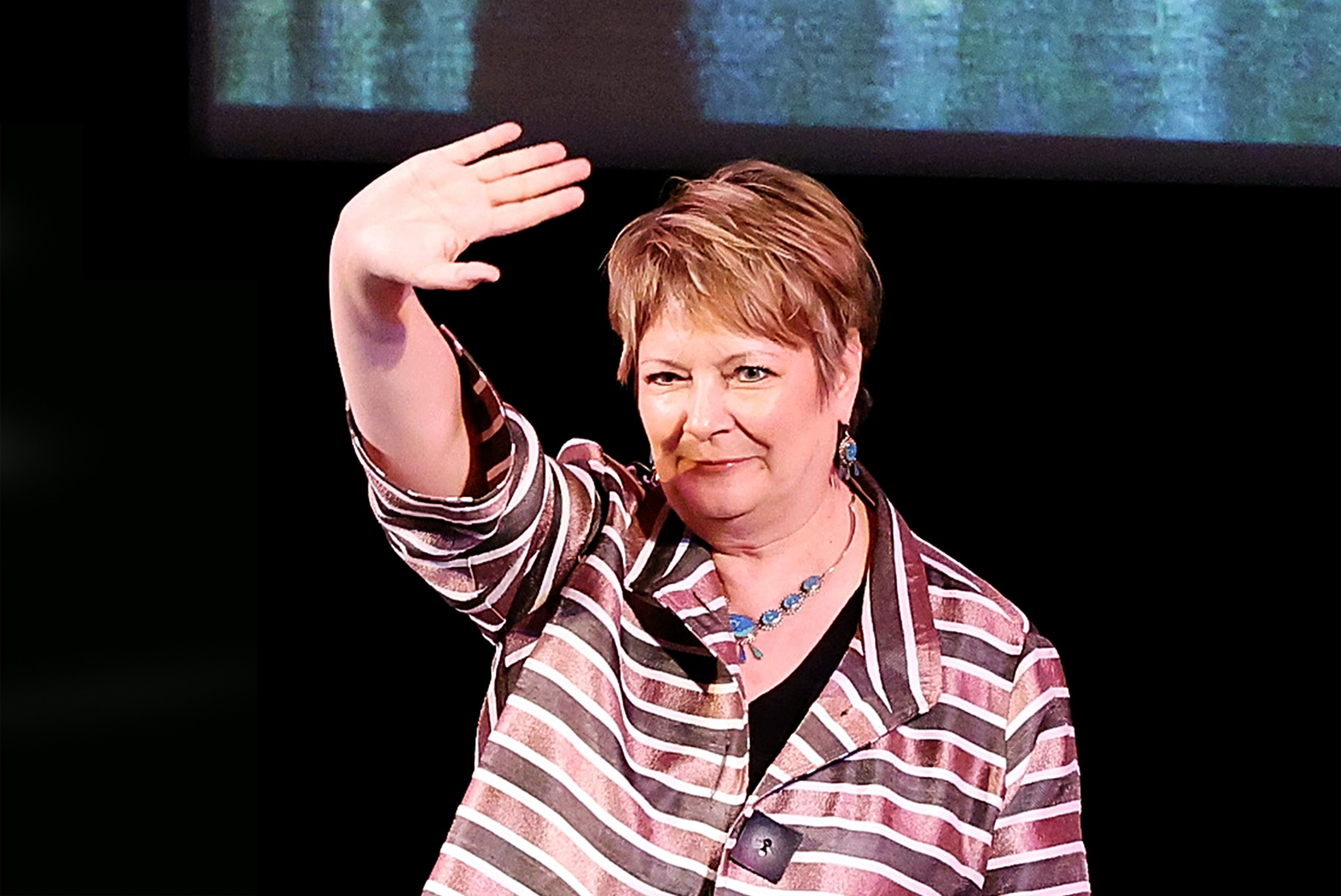
Dr. Amy Faith Ho, MD, MPH, is an emergency physician, published writer, and national speaker on issues pertaining to health care and health policy, with work featured in Forbes, Chicago Tribune, NPR, KevinMD, and TEDx.
The views expressed in this article are the writer's own.