Prone-back ECG in COVID-19 patients useful for arrhythmia detection, JACC study
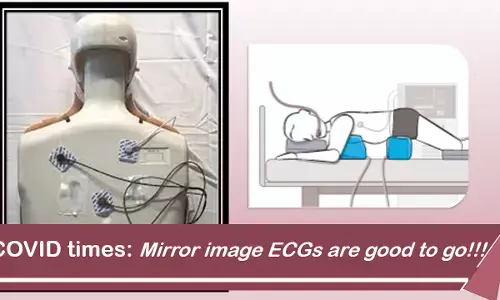

Figure 1.Comparison of supine and prone back ECGs.
How good is prone-back position ECG to detect arrhythmias and ischemic changes in these patients? According to a recent study published in JACC Clinical Electrophysiology, prone back (PB) position ECG can serve as a useful screening tool with good diagnostic utility in COVID-19 patients who require prone ventilation.
In COVID-19 patients with hypoxic respiratory failure, early intubation and ventilation including prone-position ventilation have been recommended in society guidelines. As taking a routine supine position ECG can be cumbersome in these patients, the value of a prone position ECG needs to be explored.
Here, the precordial leads are positioned posteriorly in a mirror image to usual anterior chest wall positions in 4th and 5th intercostal spaces (Figure 1). This avoids repositioning patients for a 12-lead ECG, which may result in oxygen desaturation and is labor-intensive.
Chieng et al conducted a study to describe expected changes in a mirror-image prone electrocardiogram (ECG) compared with normal supine, including a range of cardiac conditions. This prospective study was designed to:
1) Describe expected differences in the 12-lead ECG in the prone position compared with the supine and;
2) Determine the usefulness of the prone ECG in detecting myocardial injury and abnormalities in rhythm and conduction.
Hundred patients each underwent 3 ECGs: standard supine front (SF); prone position with precordial leads attached to front (PF); and prone with precordial leads attached to back in a mirror image to front (PB).
The study gave the following insights:
a) Prone positioning was associated with a numerically small, but statistically significant, QTc prolongation.
b) PB was associated with new qR morphology in leads V 1 to V 3 in 90% and a significant reduction in R-, S-, and T-wave amplitude in leads V 1 to V 3 .
c) In patients with anterior myocardial ischemia/infarct with ST changes in leads V 1 to V 3 on SF ECG, these changes were no longer visible in V 1 to V 3 on PB. By contrast, ST-segment elevation/depression in the limb leads remained mostly unchanged in the PB position.
d) PB positioning was associated with a change in the polarity of the T wave in leads V 1 to V 3 in 84%. T wave inversion in lateral precordial/limb leads remained unaffected by PB positioning.
e) LBBB demonstrated a polarity shift, with a RBBB appearance in a PB position.
f) RBBB became narrower with a qR appearance in V 1 to V 3 .
g) Arrhythmia detection was not affected by prone positioning.
ECG lead placement in a posterior body position is not a unique concept. Classically posterior leads V 7 to V 9 , have been used as an extension of precordial leads V 1 to V 6 in the detection of posterior myocardial infarction .
The PB ECG provides reliable rhythm monitoring and detection of myocardial injury involving the inferior and lateral myocardium, making it a useful alternative to the traditional supine ECG to avoid repositioning a patient who requires prone ventilation. However, the PB ECG is not reliable for the detection of anterior ischemia.
Machine learning–based prediction models could be developed to predict ECG appearances in a traditional supine front position based on the appearance of a prone back ECG.
Source: JACC CE: DOI: 10.1016/j.jacep.2021.04.011
