Lung Ultrasound helps achieve faster resolution of congestion in acute heart failure
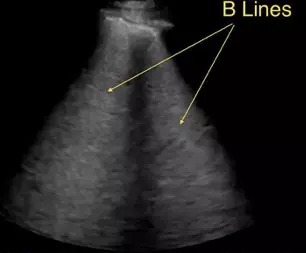
Acute heart failure (AHF) is known to be associated with poor in-hospital and post discharge outcomes. Although no initial management strategy improves outcome in such patients, initial goal of care is to address pulmonary congestion. Measurement of lung B lines by ultrasound provides semi quantitative assessment of pulmonary congestion but the response of these B lines to diuretic therapy is not well described in the literature.
Peter S. Pang et.al, conducted a randomized controlled, single-blind trial to determine if a 6-h lung ultrasound (LUS)-guided management improves pulmonary congestion over usual management guided solely by clinical reassessment in emergency setting. A secondary goal was to explore whether early targeted intervention leads to improved outcomes
This study was conducted across 4 centers in United States and included adult patients, with a history of HF, shortness of breath, and having at least one sign or radiographic evidence of AHF. Patients were required to have >15 B-lines in both hemithoraces on imaging. A total of 130 patients were randomized in 1:1 fashion.
The total number of B lines per patient at 6 hours was similar in both the groups. No differences were observed between treatment arms regarding length of hospital stay or days alive and out of hospital (DAOOH) at 30 days. A significantly greater reduction in the number of B-lines was observed in the LUS- guided arm than in the usual care arm during the first 48 hours, suggesting that LUS-guided patients had faster resolution of congestion. By the time of discharge, this difference in B-line reduction between the 2 arms was no longer significant.
Although protocol-driven treatment stopped at 6 h, repeat dosing during this interval was more common in the LUS-guided arm. This suggests that protocol-driven therapy might facilitate a more rapid reduction in congestion. Persistence of B-lines pre-discharge identifies patients at higher risk for worse outcomes.
Authors concluded saying that targeting pulmonary congestion with LUS did not show any significant decrease in pulmonary congestion within 6 hours compared with usual standard care. However, a consistent numeric reduction in pulmonary congestion, as measured by B-lines, in the intervention group was observed during hospitalization, suggesting that future work targeting B-line reduction throughout hospitalization is warranted.
Source:JACC heart failure journal