Top Searches
- News
- City News
- mumbai News
- Hospital bills not audited and 80:20 scheme under-utilized: Activists
Hospital bills not audited and 80:20 scheme under-utilized: Activists

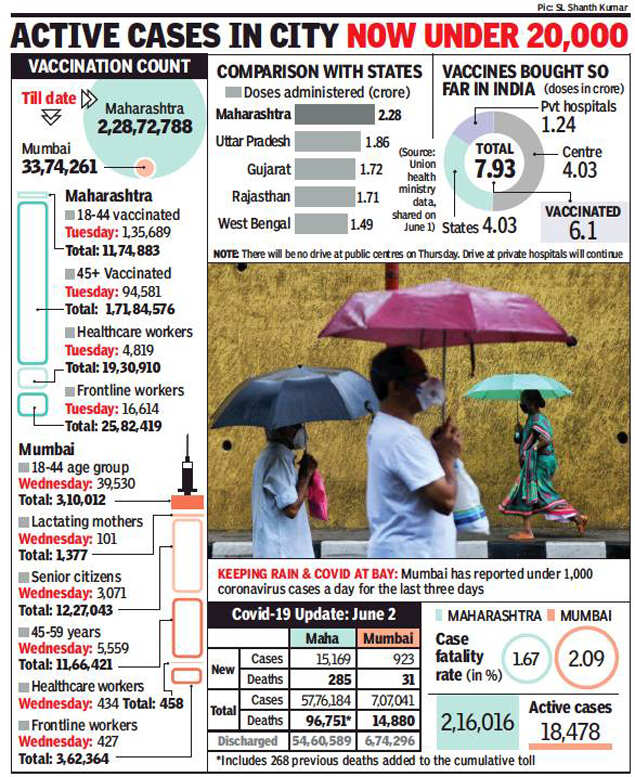
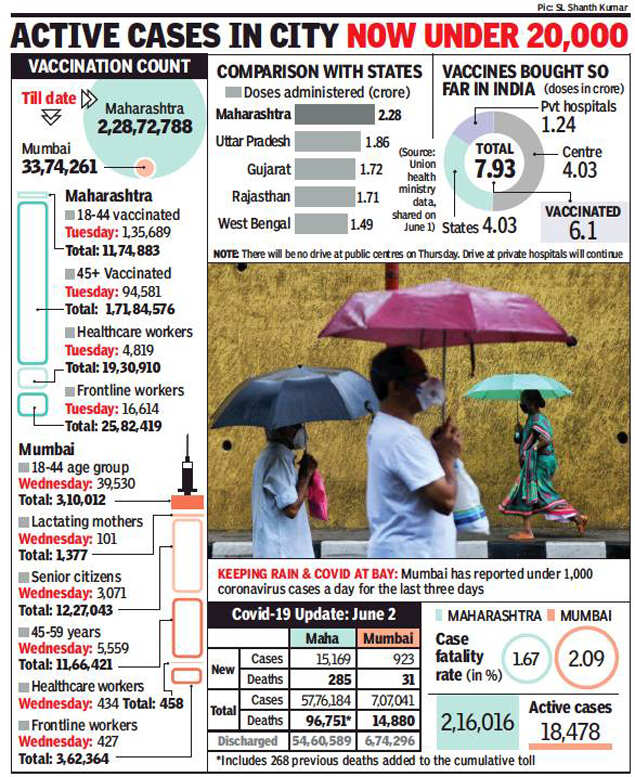
Mumbai has reported under 1,000 coronavirus cases a day for the last three days
MUMBAI: The state’s 80:20 scheme that was first in India to regulate private beds and cap charges for Covid treatment has remained underutilised in most parts of the state, according to activists. They have demanded auditing of hospital bills on a bigger scale mainly in tier-II and III cities, and efforts to popularise the scheme.
On Tuesday, the scheme was given an extension for the fifth time and will now be in force till August 31. But public health activists said without awareness, the scheme could largely remain on paper. Dr Abhijit More of Jan Swasthya Abhiyan cited the example of Pune, where less than 2% of bills have been audited. “It shows people don’t know treatment rates are capped and that they can seek an audit. 80:20 deserves wider publicity,” he said, adding the government has failed to propagate it.
TOI found out the state doesn’t possess a consolidated number of how many bills have been audited and how much money has been refunded to patients, barring from bigger districts like Mumbai, Pune, Nagpur. A state official said most local bodies have “failed” to implement the scheme. “Many haven’t designated auditors to review bills,” he said. Several districts decided to audit only bills over Rs 1.5 lakh though no such limit was suggested, the official said. The revised version mandates pre-auditing of every bill before it goes to patients.
So far, Mumbai has refunded over Rs 15.5 crore, Pune over Rs 3 crore and Nagpur nearly Rs 2 crore to patients who were charged more than what has been fixed. The rate for isolation beds under 80:20 is now Rs 2,400 to Rs 4,000, ICU without ventilator is Rs 4,500 to 7,500 and ICU with ventilator is Rs 5,400 and Rs 9,000. Charges like doctors’ consultation, routine examinations and oxygen rates are included in room rates, but patients get charged additionally.
Noted medical activist Dr Arun Gadre said the idea of such a scheme was commendable, but implementation and monitoring has faltered. He blamed private hospitals mainly for deliberately depriving people by not spelling out if the patient was being hospitalised under the 80% quota or 20%. “Under 20%, where hospitals can command their own rates, people have been charged arbitrarily, but in the absence of auditors, it went unchecked,” he said. Given that Maharashtra has not regulated the private sector for 30 years, it was expected they would find it difficult to create monitoring systems overnight, he added.
In smaller districts, awareness is abysmal, said Nanded-based Ujjwala Padalwar of ASHA Gatpravartka Federation. “When the 2nd wave hit, people were at the mercy of private hospitals and had to pay anything from Rs 20,000 to half a lakh for admission,” she said. “When people don’t know about the scheme, how will they contest the charges,” she said.
Dr Sudhakar Shinde, who was instrumental in framing the policy, said the state will work towards popularising it.
On Tuesday, the scheme was given an extension for the fifth time and will now be in force till August 31. But public health activists said without awareness, the scheme could largely remain on paper. Dr Abhijit More of Jan Swasthya Abhiyan cited the example of Pune, where less than 2% of bills have been audited. “It shows people don’t know treatment rates are capped and that they can seek an audit. 80:20 deserves wider publicity,” he said, adding the government has failed to propagate it.
TOI found out the state doesn’t possess a consolidated number of how many bills have been audited and how much money has been refunded to patients, barring from bigger districts like Mumbai, Pune, Nagpur. A state official said most local bodies have “failed” to implement the scheme. “Many haven’t designated auditors to review bills,” he said. Several districts decided to audit only bills over Rs 1.5 lakh though no such limit was suggested, the official said. The revised version mandates pre-auditing of every bill before it goes to patients.
So far, Mumbai has refunded over Rs 15.5 crore, Pune over Rs 3 crore and Nagpur nearly Rs 2 crore to patients who were charged more than what has been fixed. The rate for isolation beds under 80:20 is now Rs 2,400 to Rs 4,000, ICU without ventilator is Rs 4,500 to 7,500 and ICU with ventilator is Rs 5,400 and Rs 9,000. Charges like doctors’ consultation, routine examinations and oxygen rates are included in room rates, but patients get charged additionally.
Noted medical activist Dr Arun Gadre said the idea of such a scheme was commendable, but implementation and monitoring has faltered. He blamed private hospitals mainly for deliberately depriving people by not spelling out if the patient was being hospitalised under the 80% quota or 20%. “Under 20%, where hospitals can command their own rates, people have been charged arbitrarily, but in the absence of auditors, it went unchecked,” he said. Given that Maharashtra has not regulated the private sector for 30 years, it was expected they would find it difficult to create monitoring systems overnight, he added.
In smaller districts, awareness is abysmal, said Nanded-based Ujjwala Padalwar of ASHA Gatpravartka Federation. “When the 2nd wave hit, people were at the mercy of private hospitals and had to pay anything from Rs 20,000 to half a lakh for admission,” she said. “When people don’t know about the scheme, how will they contest the charges,” she said.
Dr Sudhakar Shinde, who was instrumental in framing the policy, said the state will work towards popularising it.
FacebookTwitterLinkedinEMail
Start a Conversation
end of article
