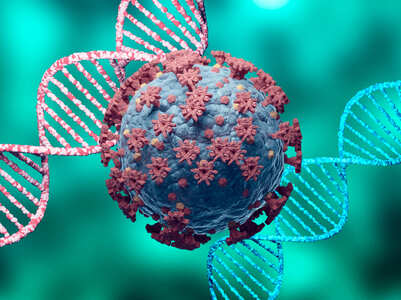
Coronavirus: How new COVID-19 variants come up and what makes it so concerning
My COVID Story: I delivered a baby while being COVID positive
The Times Of India launches '#CutTheShame' initiative to redefine narrative on menstrual health
How nicotine replacement therapy can help in quitting smoking
New Vietnam coronavirus variant: What we know so far and why we need to be careful
Coronavirus: How new COVID-19 variants come up and what makes it so concerning
Coronavirus: How new COVID-19 variants come up and what makes it so concerning

The world has been grappled with virulent strains of the SARS-COV-2 virus wreaking havoc across the world. From the strain said to have originated in Kent, UK to the much virulent double mutant virus traced in India (and now spreading across the world), mutant strains of the COVID virus are responsible for causing a lot of destruction.
However, as medical experts suggest, the current mutations may not be the most dangerous yet, or mark the end of the battle yet. In fact, there could be many more variants which may spread fear. Most recently, vaccine makers from Moderna Inc. have tried to cite caution for the world not to be complacent yet.
Read more: New symptoms to watch out for during the second COVID-19 wave
In a recent virtual conference, Moderna’s chief scientific officer, Melissa Moore was quoted saying, “As the virus spreads, it is rapidly mutating,”
Guillaume Stewart-Jones, a scientist at Moderna Therapeutics Inc. said that effective plans need to be drawn up to combat “new strains which are coming, emerging constantly in real-time”.
The news comes at a time when mRNA vaccine builds from companies like Moderna and Pfizer's offer the greatest odds of protection. It has, however, long been debated that the current vaccines under offer may only offer preventable protection 'to an extent', and booster shots may be needed to fully protect individuals from infection risks. But what exactly makes these variants prop up? And, if vaccines may not fully protect us, how do we stay safe?
Here’s all you need to know...
How do vaccine variants come up?
According to scientific research, variants of a virus come up whenever there is a change to the mutation or genetic code of the virus' strain.
By nature, viruses and many other pathogens tend to mutate and change. However, such as the case is with the virus, some variants can be genetically distinct, and cause a lot more severity. RNA viruses such as SARS-COV-2 also tend to mutate more often than other viruses.
Read more: What we know so far about the new Vietnam coronavirus variant
B.1.351 and B.1.1.7 variants, for example, which was traced around September 2020 in the UK were one of the first variants of coronavirus which propped up and to date, said to be the most predominant form of coronavirus in many countries, including India.
Each mutant or variation carries specific genetic changes which may make it more contagious or severe. For example, the B.1.1.7 variant was traced to spread easier while the double mutant variant has been found to be more severe, causing pre-lung involvement in many cases. Some variants can also attack the body in a way causing different symptoms altogether.
The prime reason as to what makes a particular variant's discovery more concerning is its ability to launch a scathing attack on the body or spread faster. It is said that virulent viruses tend to be 'smarter' and could easily surpass some of the natural antibodies, allowing them easier access to cause damage and in turn, severity.
However, it should be noted that not all virus variants are dangerous, or do harm. Only the ones genetically traced, or found to be variants of concern (VOCs) are said to be more severe in nature.
COVID-19 vaccines vs variants: What makes it so concerning
The growing rate of variants fueling the further spread of the pandemic has raised fears that the vaccines we have with us may not be much effective. A prime reason for the same can be their ability to surpass antibodies easily, which may render the vaccines rather ineffective.
However, that's not completely true. The coronavirus variants may be smarter and more severe, but the vaccines we have with us may not be completely effective. As laboratory-based studies have shown, the immune response mounted by the vaccines contain several components, and a reduction may not dim the vaccine response entirely.
Read more: Difference in onset of symptoms between the first wave and the second wave of coronavirus
How worried should we be?
Even if there are risks of future variants and mutations coming our way, vaccination, and following COVID-appropriate behaviour are some of the best ways to cut down any problematic risks. Therefore, all individuals should get their COVID-19 vaccine jabs at the earliest.
Case studies have also shown that fully vaccinated individuals have a lower threshold of suffering from severe complications, mortality risk, and in some cases, may even recover earlier. Booster shots, for example, can also be introduced to deal with future variants of concerns.
Scientists also believe that one of the best ways to test a vaccine's true efficacy would be to test them in real-world conditions and infer observations. For example, when the B.1.1.7 variant circulated in the US in early 2021, it was observed that the mRNA vaccines under offer were able to offer some protection and taper down the risk of people falling severely ill or dying from COVID-19. Similar results were seen with the Johnson and Johnson one-dose vaccine, which was about 85% effective in curbing severe disease outcomes against dominant variants prevalent in South Africa.
There are also experts who suggest that vaccination at the earliest will allow the world to minimize the spread of future variants and mitigate the risks, when and where possible. Therefore, prioritization of COVID-19 vaccination is essential. When community-level herd immunity is achieved, variants may have lower than usual chances of spreading.
However, as medical experts suggest, the current mutations may not be the most dangerous yet, or mark the end of the battle yet. In fact, there could be many more variants which may spread fear. Most recently, vaccine makers from Moderna Inc. have tried to cite caution for the world not to be complacent yet.
Read more: New symptoms to watch out for during the second COVID-19 wave
In a recent virtual conference, Moderna’s chief scientific officer, Melissa Moore was quoted saying, “As the virus spreads, it is rapidly mutating,”
Guillaume Stewart-Jones, a scientist at Moderna Therapeutics Inc. said that effective plans need to be drawn up to combat “new strains which are coming, emerging constantly in real-time”.
The news comes at a time when mRNA vaccine builds from companies like Moderna and Pfizer's offer the greatest odds of protection. It has, however, long been debated that the current vaccines under offer may only offer preventable protection 'to an extent', and booster shots may be needed to fully protect individuals from infection risks. But what exactly makes these variants prop up? And, if vaccines may not fully protect us, how do we stay safe?
Here’s all you need to know...
How do vaccine variants come up?
According to scientific research, variants of a virus come up whenever there is a change to the mutation or genetic code of the virus' strain.
By nature, viruses and many other pathogens tend to mutate and change. However, such as the case is with the virus, some variants can be genetically distinct, and cause a lot more severity. RNA viruses such as SARS-COV-2 also tend to mutate more often than other viruses.
Read more: What we know so far about the new Vietnam coronavirus variant
B.1.351 and B.1.1.7 variants, for example, which was traced around September 2020 in the UK were one of the first variants of coronavirus which propped up and to date, said to be the most predominant form of coronavirus in many countries, including India.
Each mutant or variation carries specific genetic changes which may make it more contagious or severe. For example, the B.1.1.7 variant was traced to spread easier while the double mutant variant has been found to be more severe, causing pre-lung involvement in many cases. Some variants can also attack the body in a way causing different symptoms altogether.
The prime reason as to what makes a particular variant's discovery more concerning is its ability to launch a scathing attack on the body or spread faster. It is said that virulent viruses tend to be 'smarter' and could easily surpass some of the natural antibodies, allowing them easier access to cause damage and in turn, severity.
However, it should be noted that not all virus variants are dangerous, or do harm. Only the ones genetically traced, or found to be variants of concern (VOCs) are said to be more severe in nature.
COVID-19 vaccines vs variants: What makes it so concerning
The growing rate of variants fueling the further spread of the pandemic has raised fears that the vaccines we have with us may not be much effective. A prime reason for the same can be their ability to surpass antibodies easily, which may render the vaccines rather ineffective.
However, that's not completely true. The coronavirus variants may be smarter and more severe, but the vaccines we have with us may not be completely effective. As laboratory-based studies have shown, the immune response mounted by the vaccines contain several components, and a reduction may not dim the vaccine response entirely.
Read more: Difference in onset of symptoms between the first wave and the second wave of coronavirus
How worried should we be?
Even if there are risks of future variants and mutations coming our way, vaccination, and following COVID-appropriate behaviour are some of the best ways to cut down any problematic risks. Therefore, all individuals should get their COVID-19 vaccine jabs at the earliest.
Case studies have also shown that fully vaccinated individuals have a lower threshold of suffering from severe complications, mortality risk, and in some cases, may even recover earlier. Booster shots, for example, can also be introduced to deal with future variants of concerns.
Scientists also believe that one of the best ways to test a vaccine's true efficacy would be to test them in real-world conditions and infer observations. For example, when the B.1.1.7 variant circulated in the US in early 2021, it was observed that the mRNA vaccines under offer were able to offer some protection and taper down the risk of people falling severely ill or dying from COVID-19. Similar results were seen with the Johnson and Johnson one-dose vaccine, which was about 85% effective in curbing severe disease outcomes against dominant variants prevalent in South Africa.
There are also experts who suggest that vaccination at the earliest will allow the world to minimize the spread of future variants and mitigate the risks, when and where possible. Therefore, prioritization of COVID-19 vaccination is essential. When community-level herd immunity is achieved, variants may have lower than usual chances of spreading.
End of the article
Comments (0)
Featured in Health & Fitness

How do new COVID-19 variants come up?
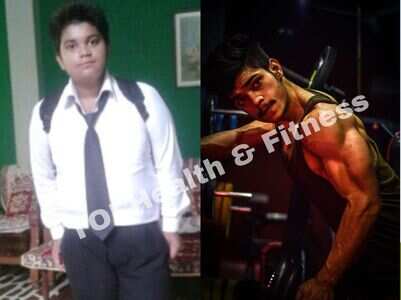
"Chapati-chicken is my big weight loss secret"

Is it safe to have kadha during summer?

My COVID: I delivered a baby while being COVID+

Types of mucormycosis observed in COVID patients

COVID symptoms that may arise post vaccination

Top zinc-rich foods you can have
New Vietnam COVID variant: What we know so far

How nicotine replacement therapy can help
LATEST VIDEOS
Health-Fitness
 Habits you must follow for fit and fine body and mind00:37
Habits you must follow for fit and fine body and mind00:37 Second-hand smoking and how we are all at risk05:34
Second-hand smoking and how we are all at risk05:34 All about antibody cocktail drug to fight COVID03:48
All about antibody cocktail drug to fight COVID03:48 Teas that will help you boost your immunity00:29
Teas that will help you boost your immunity00:29 Black fungus vs White fungus: What's the difference?00:59
Black fungus vs White fungus: What's the difference?00:59 Is black fungus infection contagious?00:59
Is black fungus infection contagious?00:59 Recovering from COVID-19? Follow these dietary guidelines05:31
Recovering from COVID-19? Follow these dietary guidelines05:31 COVID-19 recovery: 6 food tips for a speedy recovery from coronavirus05:33
COVID-19 recovery: 6 food tips for a speedy recovery from coronavirus05:33 Busting some common myths around Erectile Dysfunction 07:21
Busting some common myths around Erectile Dysfunction 07:21 Lemon tea is beneficial for your body00:41
Lemon tea is beneficial for your body00:41
StoriesSEE All





























































































![[New!] Level 4 - 30 minute tempo fat-burning!
[New!] Level 4 - 30 minute tempo fat-burning!](https://static.toiimg.com/thumb/79327298.cms?width=147&height=86)













closecomments
SIGN IN WITH
FacebookGoogleEmail