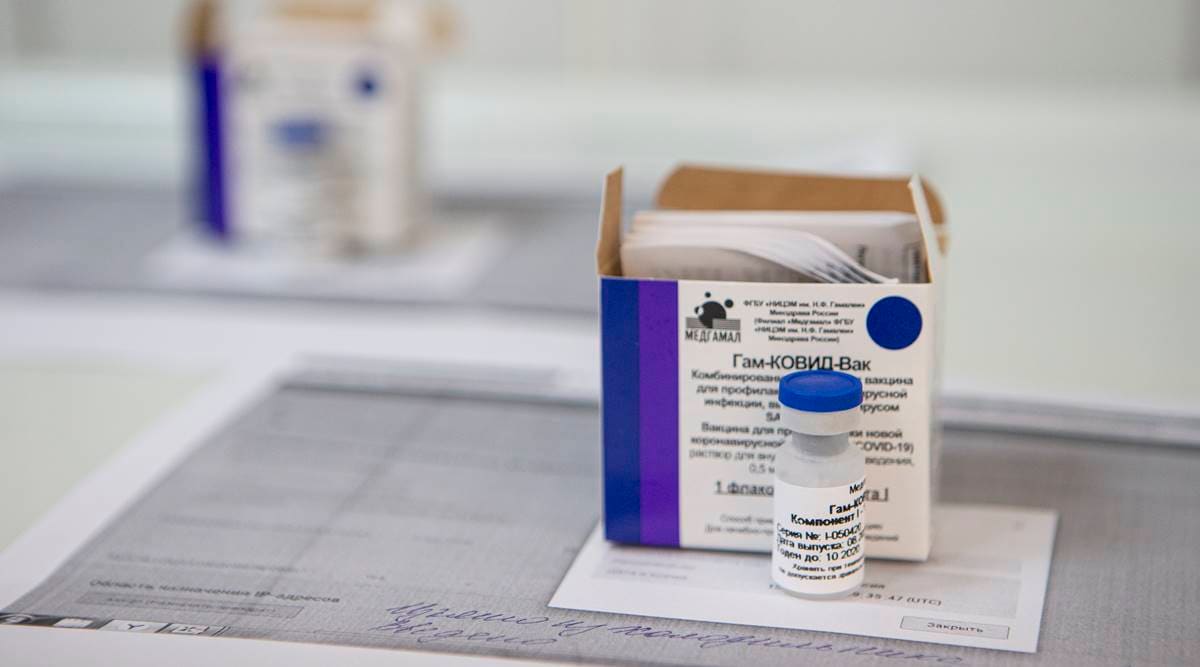
 A view of a vial of Russia's experimental Sputnik V coronavirus vaccine. (Photo: AP)
A view of a vial of Russia's experimental Sputnik V coronavirus vaccine. (Photo: AP)Written by Amir Ullah Khan
In 2012, in Saudi Arabia, a novel deadly respiratory virus was recorded, where the infection led to the death of every third patient. The clinical picture was typical for an acute respiratory viral disease — the first symptoms were fever, cough, shortness of breath, which, as the disease progressed, turned into severe viral pneumonia, which eventually caused death. The virus, subsequently called the Middle East Respiratory syndrome (MERS), soon spread beyond Saudi Arabia to the entire Middle Eastern region, Europe and Asia-Pacific with 27 countries, including the United States. However, the MERS outbreak did not turn into a pandemic — as of 2020, we have seen only 2,506 cases registered globally with a total of 912 deaths. The reason for this moderate spread of the MERS virus was because it was less contagious than the novel coronavirus and only close contact with the patient could lead to infection.
In stark contrast, COVID-19, the novel virus from the same coronavirus family, while not as deadly as MERS in all cases is far more contagious. The outbreak that began in December 2019 in the Chinese province of Wuhan has already resulted in more than 41 million cases and about 1.2 million reported deaths. The spread of the disease, which has similar symptoms to MERS, has not been stopped, however, the developments undertaken to combat MERS could be crucial in the fight against COVID-19.
The role that Russia has played has not yet been discussed completely. While the country has been criticised for registering a vaccine so quickly, its adenovirus vector-based platform has been tested on thousands of people across the world over the last few decades. The COVID-19 vaccine is estimated to be remarkably like the MERS vaccine that was ready after trials before the current pandemic in Russia. On the contrary, vaccines developed elsewhere, which use chimpanzee adenoviruses as a platform and are DNA- and mRNA-based are relatively untested and will require more tests and clinical trials.
The development of a vaccine against the virus can become a turning point in overcoming the global pandemic. Today, such a vaccine is being developed by the world’s leading countries, including the United States, Great Britain, China and Russia. The main types of vaccines in development include vector, inactivated, DNA- and mRNA-based and recombinant protein-based vaccines. Developing a new vaccine normally takes at least one-and-a-half years as it requires conducting full-scale clinical trials, involving thousands of people. The devastation caused by the pandemic demands a swift response and Russian scientists from the Gamaleya Research Institute of Epidemiology and Microbiology have proposed an alternative mechanism – to create a vaccine against COVID-19 based on an existing platform that has been properly tested and proven to be safe and effective.
The Russian vaccine, Sputnik V, is an adenovirus-vector-based vaccine, and these types of medications are considered extremely safe, and straightforward to engineer. The technological platform has been studied in the development of vaccines against other infections such as the Ebola virus as well as MERS. After the start of the pandemic, a fragment of genetic material from the novel coronavirus, which codes information about the structure of the spike S-protein and forms the virus’ “crown”, was extracted. The material was inserted into a familiar adenovirus vector for delivery into a human cell creating the COVID-19 vaccine.
Vectors are viruses that have had the gene responsible for replication removed and no longer pose any threat of infection. Scientists use vectors to transport genetic material from a different virus — the one that is being vaccinated against — into a human cell. More than 20,000 people around the world have participated in clinical trials on drugs that use adenovirus vectors. Today, many countries are developing their own vaccines based on adenoviruses, but one of the fundamental differences between the Russian vaccine and other candidates is its two-shot model.
The vaccine uses a two-shot model with two different human adenoviral vectors, Ad5 and Ad26, for each shot. In this way, two different adenoviral vectors trick the body, which has the effect of causing the body to develop immunity against the first type of vector and subsequently through the second shot (using a different vector), boosts the effect of the vaccine.
During the first vaccination, a vector with a gene coding S-protein of coronavirus reaches a cell, making the body synthesize S-protein in response – at this stage, immunity is being activated. The second vaccination takes place 21 days after the initial one. The vaccine based on another adenovirus vector unknown to the body further boosts the immune response and provides for long-lasting immunity.
The Lancet has recently published the outcomes of clinical trials of Phase I-II of this vaccine, discussing its safety and efficacy. Clinical trials of this vaccine have demonstrated positive results with 100 per cent of volunteers developing a strong immunity response with no reported side-effects. Volunteers have developed a strong immune response within 21 days, and after the second shot, the number of antibodies produced by the body doubled, providing long-lasting immunity.
While the first results look encouraging, the medical community expects to see the initial results of final clinical trials as soon as November. It is now undergoing the final stage of large-scale clinical trials involving 40,000 of people across the globe, which should provide the world with a better understanding of how effective the Russian vaccine is and whether it has a fair chance of becoming the main weapon in the global war against the pandemic.
The writer is an economist at the MCRHRDI of the Government of Telangana.