BENGALURU: A team of researchers from the Centre for BioSystems Science and Engineering (BSSE) and the Department of Molecular Reproduction, Development and Genetics (MRDG) at the Indian Institute of Science (IISc) has developed a non-invasive bandage made with magnetic nanofibres to treat skin cancer by administering heat to the tumour cells.
Although this novel treatment has been shown to be effective against skin cancer in lab experiments, it is still at a nascent stage of development as a clinical therapy. IISc said that further studies are required to test the efficacy of this method on a larger scale in rabbits, dogs, and monkeys before employing it for pre-clinical and clinical applications.
Skin cancer, the most common kind of cancer, is caused mainly due to excessive exposure to ultraviolet rays from Sun.
Pointing out that the common treatments for skin cancer — surgery, radiation therapy, and chemotherapy — and other conventional therapies have limitations, IISc said in a statement that a promising alternative that has emerged to treat skin cancer is hyperthermia, which involves applying heat to the affected tissues.
“In recent years, researchers have been working on developing ways of delivering heat to the tumour tissues so that cancer cells are targeted selectively and effectively. One such technology is called magnetic hyperthermia, in which magnetic nanoparticles are used to heat the tumours by using an external alternating current magnetic field (AMF),” IISc said.
Having found that it was difficult to achieve uniform heating of the affected tissues using such magnetic nanoparticles because of uncontrolled aggregation and given that they can accumulate in the human body and induce toxicity, BSSE and MRDG researchers developed the bandage with a unique blend of magnetic nanoparticles fabricated using a method called electrospinning.
“...It comprises nanoparticles made from an oxide of iron, Fe3O4, and a biodegradable polymer called polycaprolactone (PCL) pasted on a surgical tape. The magnetic material generates heat when it is subjected to a high-frequency oscillating magnetic field,” the statement read,
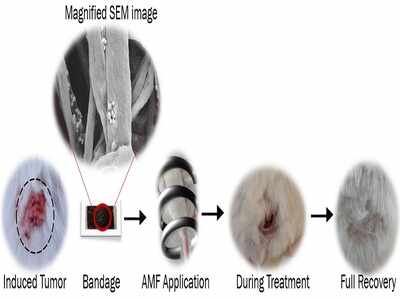
In order to investigate whether the heat generated and dissipated by the magnetic bandage can treat skin cancer, researchers did two experiments: one was in vitro (on human cancer cell lines) and the other was in vivo (on mice with artificially-induced skin cancer).
“The protocol used to prepare the PCL-Fe3O4 fibrous mat-based bandage took a little more than two months to optimise; however, the in vitro and in vivo tests that involved testing of the magnetic thermal therapy took quite some time to optimise,” Kaushik Suneet, a former project associate at BSSE and the first author of the study, said.
In both experiments, the heat generated by applying AMF to the nanofibrous magnetic bandage killed cancer cells successfully. Moreover, in the in vivo experiment, the healthy tissue remained intact with no signs of burns, inflammation, or thickening.
“The elevated temperature at the treatment site enables heat to penetrate the tumour cells, rupturing the compact random vasculatures (network of blood vessels) of tumours,” explains Shilpee Jain, who was a DST-INSPIRE Faculty Fellow at BSSE when the study was conducted, and is a senior author of the paper.
In contrast, the normal healthy cells, owing to their organised open vasculatures, dissipate the heat to maintain normal temperatures, and so remain unharmed.
Although this novel treatment has been shown to be effective against skin cancer in lab experiments, it is still at a nascent stage of development as a clinical therapy. IISc said that further studies are required to test the efficacy of this method on a larger scale in rabbits, dogs, and monkeys before employing it for pre-clinical and clinical applications.
Skin cancer, the most common kind of cancer, is caused mainly due to excessive exposure to ultraviolet rays from Sun.
Pointing out that the common treatments for skin cancer — surgery, radiation therapy, and chemotherapy — and other conventional therapies have limitations, IISc said in a statement that a promising alternative that has emerged to treat skin cancer is hyperthermia, which involves applying heat to the affected tissues.
“In recent years, researchers have been working on developing ways of delivering heat to the tumour tissues so that cancer cells are targeted selectively and effectively. One such technology is called magnetic hyperthermia, in which magnetic nanoparticles are used to heat the tumours by using an external alternating current magnetic field (AMF),” IISc said.
Having found that it was difficult to achieve uniform heating of the affected tissues using such magnetic nanoparticles because of uncontrolled aggregation and given that they can accumulate in the human body and induce toxicity, BSSE and MRDG researchers developed the bandage with a unique blend of magnetic nanoparticles fabricated using a method called electrospinning.
“...It comprises nanoparticles made from an oxide of iron, Fe3O4, and a biodegradable polymer called polycaprolactone (PCL) pasted on a surgical tape. The magnetic material generates heat when it is subjected to a high-frequency oscillating magnetic field,” the statement read,
In order to investigate whether the heat generated and dissipated by the magnetic bandage can treat skin cancer, researchers did two experiments: one was in vitro (on human cancer cell lines) and the other was in vivo (on mice with artificially-induced skin cancer).
“The protocol used to prepare the PCL-Fe3O4 fibrous mat-based bandage took a little more than two months to optimise; however, the in vitro and in vivo tests that involved testing of the magnetic thermal therapy took quite some time to optimise,” Kaushik Suneet, a former project associate at BSSE and the first author of the study, said.
In both experiments, the heat generated by applying AMF to the nanofibrous magnetic bandage killed cancer cells successfully. Moreover, in the in vivo experiment, the healthy tissue remained intact with no signs of burns, inflammation, or thickening.
“The elevated temperature at the treatment site enables heat to penetrate the tumour cells, rupturing the compact random vasculatures (network of blood vessels) of tumours,” explains Shilpee Jain, who was a DST-INSPIRE Faculty Fellow at BSSE when the study was conducted, and is a senior author of the paper.
In contrast, the normal healthy cells, owing to their organised open vasculatures, dissipate the heat to maintain normal temperatures, and so remain unharmed.
Download
The Times of India News App for Latest India News

Coronavirus outbreak
Trending Topics
LATEST VIDEOS
India
 IAF Day 2020: Apache and Chinook helicopters steal show at Hindon Air Base
IAF Day 2020: Apache and Chinook helicopters steal show at Hindon Air Base  Watch how Rafale fighter aircraft forms a figure of eight on the 88th IAF day
Watch how Rafale fighter aircraft forms a figure of eight on the 88th IAF day  IAF Day 2020: We will be ready to safeguard India’s sovereignty, says IAF chief RKS Bhadauria
IAF Day 2020: We will be ready to safeguard India’s sovereignty, says IAF chief RKS Bhadauria  Former CBI director Ashwani Kumar dies by suicide in Shimla
Former CBI director Ashwani Kumar dies by suicide in Shimla  Former CBI director Ashwani Kumar found hanging
Former CBI director Ashwani Kumar found hanging  Protesters can’t block roads or public spaces, rules Supreme Court
Protesters can’t block roads or public spaces, rules Supreme Court
More from TOI
Navbharat Times
Featured Today in Travel
Quick Links
Coronavirus in MumbaiCoronavirus in KolkataCoronavirus in HyderabadCoronavirus in DelhiCoronavirus in BangaloreCoronavirus symptomsCoronavirus in IndiaWhat is CoronavirusCoronavirus NewsSolar EclipseNPRWhat is NRCCAB BillCAB and NRCRTI BillPodcast newsLok SabhaShiv SenaYSRCPCongressBJP newsUIDAIIndian ArmyISRO newsSupreme Court
Get the app



