
Seated in his Mira Road home, Mohsin Khan tapped his cellphone and his south Mumbai gastroenterologist popped up on the screen. Following a brief chat, as the awkwardness melted, Khan saw his phone transform into a do-it-yourself medical tool as the doctor-on-camera guided Khan's finger to move up, down, poke and prod his own abdomen before sending out a photograph of the handwritten and signed prescription on his official notepad. The routine took 10 minutes and Khan recovered two days later.
"It did feel strange at first," said Khan, who missed the "doctor's touch" to check his pulse or peer into his mouth for telltale signs. But a lot could still be accomplished over video, he said. "At a time when you can't risk sitting for hours in a waiting room where another patient might transmit the coronavirus, it's a huge relief."
Khan is among a growing number of people switching to audio-visual technology to "visit" a doctor as coronavirus renders hospitals and doctor's chambers no-go zones.
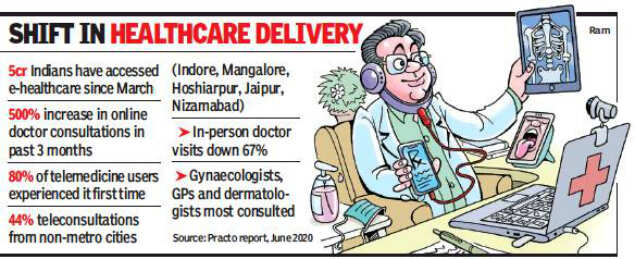
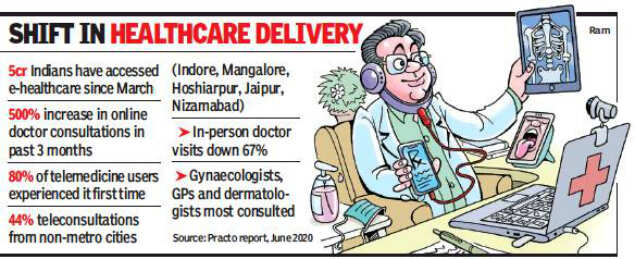
Developed a long ago, telemedicine has finally taken off during the pandemic. A private study showed up to 80% were first-time users.
Doctors trained in virtual calls, patients in uploading reports
Developed decades ago to serve far-flung rural areas, virtual healthcare, also called telemedicine, digital health, or remote care over video, phone and web-based platforms, has found a fresh lease of life during this pandemic.
Taking heed, healthcare providers are rapidly laying the ground for clinics on the cloud.
With artificial intelligence at the core of these virtual visits, Mahim’s P D Hinduja Hospital developed its own teleconsultation software that it launched in April, shortly after the lockdown while in February Apollo Hospitals launched Apollo 247, a virtual consultation platform that provides round-the-clock access to their doctors over video, audio or text. If the in-house technology team at H N Reliance Hospital in Girgaon helped familiarize doctors with their virtual OPD, doctors at Hinduja had to undergo a three- day training on handling audio, video and chat, including mock calls. Virtual platforms have been handling 200 to 1,000 virtual calls in a day with gynaecologists, GPs and dermatologists being the top draw.
A video call can last five minutes to 20 after a patient schedules an appointment with a doctor of choice and pays the charges for a virtual consultation mandated to be the same as physical. Before the virtual visit, they receive a call explaining the log-in process and how to upload past medical records, scans and prescriptions.
For Dr Rahul Gupta, a senior cardiologist with Apollo Hospitals, preparing for a video appointment with a patient is a lot like setting up a television broadcast. “A different level of care and etiquette is needed during remote consultations. For instance, eye contact is important. That’s the reason why I had to adjust the lighting in a way so they feel connected when I’m looking at them and helps me appear fresh and bright on the webcam. A dim, dark and cluttered environment can be unsettling.”
Older adults, though, may find it difficult to navigate, says Vishakha Kamat from Vile Parle who recently helped her septuagenarian mother interact with her nephrologist.
The origin of telemedicine can be traced to 2000 when the Indian Space Research Organization made a modest beginning with a pilot project using satellite communication to link Chennai’s Apollo Hospital with a rural one in the Chittoor district of Andhra Pradesh. Over the next few years, ISRO’s telemedicine facilities helped the government and some private players connect offshore islands and remote districts with major specialty hospitals in the cities.
Despite being around for close to two decades, virtual healthcare remained in a nascent state, given the ambiguities around legislation. This year, Medical Council of India permitted telemedicine by registered doctors and released guidelines on March 25, prepared in partnership with NITI Aayog. “MCI is in the process of developing an online telemedicine course, which will be mandatory for all medical practitioners after three years to tele-consult in future,” says Maharashtra Medical Council president Dr Shivkumar Utture. (Patient names changed)
"It did feel strange at first," said Khan, who missed the "doctor's touch" to check his pulse or peer into his mouth for telltale signs. But a lot could still be accomplished over video, he said. "At a time when you can't risk sitting for hours in a waiting room where another patient might transmit the coronavirus, it's a huge relief."
Khan is among a growing number of people switching to audio-visual technology to "visit" a doctor as coronavirus renders hospitals and doctor's chambers no-go zones.
Developed a long ago, telemedicine has finally taken off during the pandemic. A private study showed up to 80% were first-time users.
Doctors trained in virtual calls, patients in uploading reports
Developed decades ago to serve far-flung rural areas, virtual healthcare, also called telemedicine, digital health, or remote care over video, phone and web-based platforms, has found a fresh lease of life during this pandemic.
Taking heed, healthcare providers are rapidly laying the ground for clinics on the cloud.
With artificial intelligence at the core of these virtual visits, Mahim’s P D Hinduja Hospital developed its own teleconsultation software that it launched in April, shortly after the lockdown while in February Apollo Hospitals launched Apollo 247, a virtual consultation platform that provides round-the-clock access to their doctors over video, audio or text. If the in-house technology team at H N Reliance Hospital in Girgaon helped familiarize doctors with their virtual OPD, doctors at Hinduja had to undergo a three- day training on handling audio, video and chat, including mock calls. Virtual platforms have been handling 200 to 1,000 virtual calls in a day with gynaecologists, GPs and dermatologists being the top draw.
A video call can last five minutes to 20 after a patient schedules an appointment with a doctor of choice and pays the charges for a virtual consultation mandated to be the same as physical. Before the virtual visit, they receive a call explaining the log-in process and how to upload past medical records, scans and prescriptions.
For Dr Rahul Gupta, a senior cardiologist with Apollo Hospitals, preparing for a video appointment with a patient is a lot like setting up a television broadcast. “A different level of care and etiquette is needed during remote consultations. For instance, eye contact is important. That’s the reason why I had to adjust the lighting in a way so they feel connected when I’m looking at them and helps me appear fresh and bright on the webcam. A dim, dark and cluttered environment can be unsettling.”
Older adults, though, may find it difficult to navigate, says Vishakha Kamat from Vile Parle who recently helped her septuagenarian mother interact with her nephrologist.
The origin of telemedicine can be traced to 2000 when the Indian Space Research Organization made a modest beginning with a pilot project using satellite communication to link Chennai’s Apollo Hospital with a rural one in the Chittoor district of Andhra Pradesh. Over the next few years, ISRO’s telemedicine facilities helped the government and some private players connect offshore islands and remote districts with major specialty hospitals in the cities.
Despite being around for close to two decades, virtual healthcare remained in a nascent state, given the ambiguities around legislation. This year, Medical Council of India permitted telemedicine by registered doctors and released guidelines on March 25, prepared in partnership with NITI Aayog. “MCI is in the process of developing an online telemedicine course, which will be mandatory for all medical practitioners after three years to tele-consult in future,” says Maharashtra Medical Council president Dr Shivkumar Utture. (Patient names changed)

Coronavirus outbreak
Trending Topics
LATEST VIDEOS
City
 Shocking: Son bangs on the doors of a hospital in UP, but no one opens the door; accident victim dies
Shocking: Son bangs on the doors of a hospital in UP, but no one opens the door; accident victim dies  Covid-19 crisis: Complete lockdown from Saturday 8pm to 5am on Monday in Bengaluru
Covid-19 crisis: Complete lockdown from Saturday 8pm to 5am on Monday in Bengaluru  Pune man dons mask made of gold worth almost Rs 3 lakh
Pune man dons mask made of gold worth almost Rs 3 lakh  Covid-19: Kolkata stops flights from six major cities including Delhi between July 6 and 19
Covid-19: Kolkata stops flights from six major cities including Delhi between July 6 and 19
More from TOI
Navbharat Times
Featured Today in Travel
Get the app





