https://www.timesunion.com/news/article/How-long-do-you-need-to-overcome-opioid-13017499.php
https://www.timesunion.com/news/article/How-long-do-you-need-to-overcome-opioid-13017499.php
Is six months key to overcoming opioid addiction?
A new survey of Capital Region providers, agencies offers insight into treatment gaps
Updated 9:05 pm, Friday, June 22, 2018
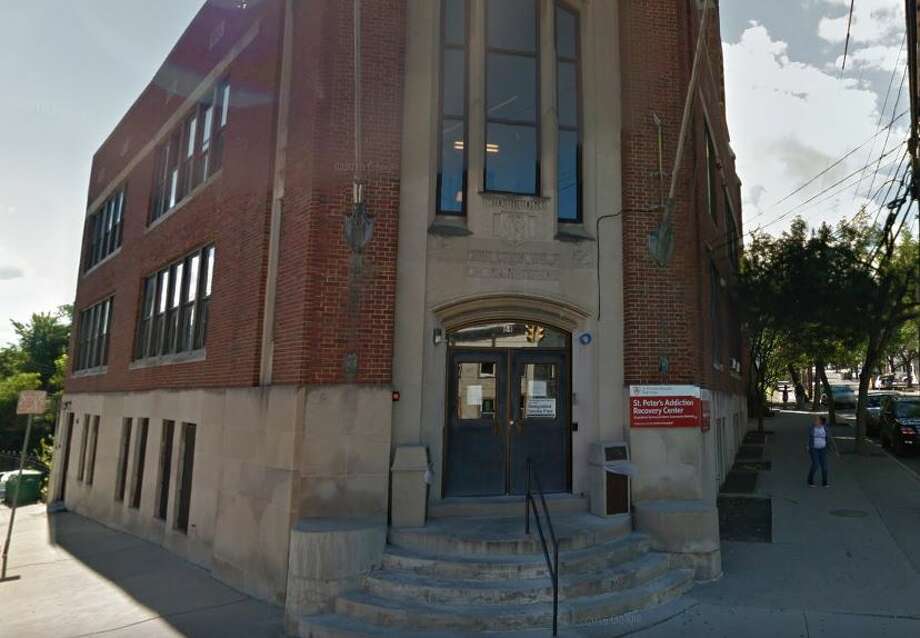
Sparc, St Peter's Addiction Recovery Center
Sparc, St Peter's Addiction Recovery Center
Three months before he died, McKinley told his mom he was ready for help, and she called and got him on a waiting list at a rehab facility in Utica. Right before he died, she learned a bed would available the next week. Learn more.
lessThree months before he died, McKinley told his mom he was ready for help, and she called and got him on a waiting list at a rehab facility in Utica. Right before he died, she learned a bed would available the
... moreAn hour before Julie Roy's son, 26-year-old William John Timber, died from a drug overdose in 2015, he hugged her and told her "I love you" – twice.
An hour before Julie Roy's son, 26-year-old William John Timber, died from a drug overdose in 2015, he hugged her and told her "I love you" – twice.
More than two years after her son's death, Roy can count all the ways the world failed him – from doctors who wouldn't prescribe medication for his withdrawal, an emergency room that turned him away for not being sick enough, an insurance plan that paid for rehab just long enough to get him clean but not a minute more, to a judge who ignored a probation officer's recommendation for intensive, inpatient, longterm help. Read more.
lessMore than two years after her son's death, Roy can count all the ways the world failed him – from doctors who wouldn't prescribe medication for his withdrawal, an emergency room that turned him away for not
... moreSaratoga County ex-cop Fred Scheidt worked with family and friends to find his daughter's heroin supplier after her overdose death in 2014. The investigation led to a former classmate, who is now serving a 10-year sentence at a federal prison in New Jersey.
lessSaratoga County ex-cop Fred Scheidt worked with family and friends to find his daughter's heroin supplier after her overdose death in 2014. The investigation led to a former classmate, who is now serving a
... moreKatie-Lynn Scheidt overdosed on heroin in early October 2014. The man who sold it to her was sentenced to 10 years in federal prison. Learn more. (Courtesy Fredrick Scheidt)
Katie-Lynn Scheidt overdosed on heroin in early October 2014. The man who sold it to her was sentenced to 10 years in federal prison. Learn more. (Courtesy Fredrick Scheidt)
Roughly five years later, Livingston is now a peer recovery advocate and director of Hope and Healing Recovery Community Center in Hudson Falls. Read her story.
Roughly five years later, Livingston is now a peer recovery advocate and director of Hope and Healing Recovery Community Center in Hudson Falls. Read her story.
In 2015 Bryan Prinz, 25, and his girlfriend, Elise Ainsworth, 20, who met in a 12-step support group in Troy, are both taking classes at Hudson Valley Community College and repairing the damage their addictions inflicted. Read their story. (John Carl D'Annibale / Times Union)
lessIn 2015 Bryan Prinz, 25, and his girlfriend, Elise Ainsworth, 20, who met in a 12-step support group in Troy, are both taking classes at Hudson Valley Community College and repairing the damage their addictions
... moreSean Murdick, left, and his brother, Tim. Read Sean's story.
Sean Murdick, left, and his brother, Tim. Read Sean's story.
Matthew Kirshner, who has been described as an "arrogant jerk," discusses his drug arrest with Table Hopping writer Steve Barnes. Kirshner was arrested on a drug charge earlier this year, served jail time and is beginning his recovery. Photographed Friday, June 1, 2018, at Stacks Espresso Bar in Albany. (Steve Barnes/Times Union.) Read the story here.
lessMatthew Kirshner, who has been described as an "arrogant jerk," discusses his drug arrest with Table Hopping writer Steve Barnes. Kirshner was arrested on a drug charge earlier this year, served jail time and
... moreMcKenna started writing a memoir in prison at the suggestion of a therapist. The result was, "Sheer Madness: From Federal Prosecutor to Federal Prisoner." As of 2015, he had been out of prison for three years and had been clean for nine years. Read his story. (Cindy Schultz / Times Union)
lessMcKenna started writing a memoir in prison at the suggestion of a therapist. The result was, "Sheer Madness: From Federal Prosecutor to Federal Prisoner." As of 2015, he had been out of prison for three years
... moreIn 2014, Naomi and Gwyn, both recovering in an adolescent residential treatment program at Hope House, shared their stories. Read more.
In 2014, Naomi and Gwyn, both recovering in an adolescent residential treatment program at Hope House, shared their stories. Read more.
In 2014, Kevin and Diane Flood's son, Dan, had battled heroin addiction for more than 6 years and had been homeless in Albany for several months. Read their story. (Lori Van Buren / Times Union)
In 2014, Kevin and Diane Flood's son, Dan, had battled heroin addiction for more than 6 years and had been homeless in Albany for several months. Read their story. (Lori Van Buren / Times Union)
Retired police officer Patty Farrell's daughter, Laree, died of a heroin overdose in her home in 2013. Read her story. (Will Waldron/Times Union)
Retired police officer Patty Farrell's daughter, Laree, died of a heroin overdose in her home in 2013. Read her story. (Will Waldron/Times Union)
Former dirt-track racer Emmanuel Donato was a heroin addict, dealer and prison convict. Read his story. (Michael P. Farrell/Times Union)
Former dirt-track racer Emmanuel Donato was a heroin addict, dealer and prison convict. Read his story. (Michael P. Farrell/Times Union)
In 2014, Donato is seen studying to be a personal trainer with a little distraction from his dog Pistol. His goal is to specialize in working with troubled youths. "I want to try to get to them before they make the mistakes I made." Read his story. (Lori Van Buren / Times Union)
lessIn 2014, Donato is seen studying to be a personal trainer with a little distraction from his dog Pistol. His goal is to specialize in working with troubled youths. "I want to try to get to them before they make
... moreEmmanuel Donato attends a group therapy session with director of counseling, Michael Ballester, right, at Equinox in 2014. Read his story. (Michael P. Farrell/Times Union)
Emmanuel Donato attends a group therapy session with director of counseling, Michael Ballester, right, at Equinox in 2014. Read his story. (Michael P. Farrell/Times Union)
in 2014, Hope House admitted Linsley anyway. "The way he was using, he wasn't long for this world," said Linda Tymeson, director of program support services. Read more. (Paul Buckowski / Times Union)
in 2014, Hope House admitted Linsley anyway. "The way he was using, he wasn't long for this world," said Linda Tymeson, director of program support services. Read more. (Paul Buckowski / Times Union)
When Therese McHale was 17 and struggling with heroin addiction, her parents' insurance plan allowed her a two-day stay at a 28-day program. It wasn't enough time, and she went back home and started using heroin again. A few months later, insurance denied another program. She was eventually arrested for a drug-related crime and was mandated a 9-month residential treatment program, which she completed successfully. Read more about heroin and insurance. (Paul Buckowski / Times Union)
lessWhen Therese McHale was 17 and struggling with heroin addiction, her parents' insurance plan allowed her a two-day stay at a 28-day program. It wasn't enough time, and she went back home and started using
... moreLyman's mother, Brenda Auerbach, stands with a photo of her son. Read more. (Michael P. Farrell/Times Union)
Lyman's mother, Brenda Auerbach, stands with a photo of her son. Read more. (Michael P. Farrell/Times Union)
Brother and sister Jeremiah and Jessica Lyman, shown here in 2010. "Heroin ruined my life, too, because it took my brother," said his sister. Read more. (Courtesy of Lyman family)
Brother and sister Jeremiah and Jessica Lyman, shown here in 2010. "Heroin ruined my life, too, because it took my brother," said his sister. Read more. (Courtesy of Lyman family)
Drug-sniffing Labrador retriever Willy works with David Harrington of Specialized K9 Detection Service, which can help parents, business owners or anyone else locate drugs on their property. Read his story.(Cindy Schultz / Times Union)
lessDrug-sniffing Labrador retriever Willy works with David Harrington of Specialized K9 Detection Service, which can help parents, business owners or anyone else locate drugs on their property. Read his
... moreDavid Harrington of Specialized K9 Detection Service and his Labrador retriever Stone prepare to search a home for drugs. Read more. (Cindy Schultz / Times Union)
David Harrington of Specialized K9 Detection Service and his Labrador retriever Stone prepare to search a home for drugs. Read more. (Cindy Schultz / Times Union)
Rensselaer County Sheriff's Deputy Zachary Sharpe talks about reviving a man from a heroin overdose using Naloxone, a relatively new opioid antagonist. Sharpe said that had he gotten to the house any later, the man likely would have died. Read his story.
lessRensselaer County Sheriff's Deputy Zachary Sharpe talks about reviving a man from a heroin overdose using Naloxone, a relatively new opioid antagonist. Sharpe said that had he gotten to the house any later, the
... moreRensselaer County Sheriff's Deputy Zachary Sharpe uses a dummy to demonstrate how to use Naloxone to revive a person from a heroin overdose. Read his story. (Bryan Fitzgerald/Times Union)
Rensselaer County Sheriff's Deputy Zachary Sharpe uses a dummy to demonstrate how to use Naloxone to revive a person from a heroin overdose. Read his story. (Bryan Fitzgerald/Times Union)
Driver Rudy Jahn stands with EMTs Carolyn Fleming and Paul Glasser who are holding the drug Naloxone Hydrochloride in 2012. The Hoags Corners EMTs were the first in a pilot program that allows EMTs to administer a drug that can reverse an opioid overdose. Read more. (Lori Van Buren / Times Union)
lessDriver Rudy Jahn stands with EMTs Carolyn Fleming and Paul Glasser who are holding the drug Naloxone Hydrochloride in 2012. The Hoags Corners EMTs were the first in a pilot program that allows EMTs to
... moreOrlando Hernandez, right, uses a bull horn to organize a march by an addiction treatment and recovery advocacy group in 2014 at the Emmanuel Baptist Church before they marched to the Capitol. Read more about heroin and insurance. (Skip Dickstein / Times Union)
lessOrlando Hernandez, right, uses a bull horn to organize a march by an addiction treatment and recovery advocacy group in 2014 at the Emmanuel Baptist Church before they marched to the Capitol. Read more about
... moreSherri Roff, left, clinical director for The Next Step, and Marsha Penrose, executive director, believe in single-gender addiction treatment. Recovery from drug abuse requires a reckoning with past behavior, a brutal honesty with oneself and others. As Roff points out, that doesn't work if a resident is trying to flirt and impress. Here they are seen in the group counseling room. Women who are graduating the program write a message on the wall of the room. They know that other women will sit in this room and read what is on the walls. Read more. (Paul Buckowski / Times Union)
lessSherri Roff, left, clinical director for The Next Step, and Marsha Penrose, executive director, believe in single-gender addiction treatment. Recovery from drug abuse requires a reckoning with past behavior, a
... moreMicky Jimenez, regional director of Capital District Camino Nuevo, said she wants clients to feel they are being embraced by la familia, whatever their background. Read more about Camino Nuevo. (Paul Buckowski / Times Union)
lessMicky Jimenez, regional director of Capital District Camino Nuevo, said she wants clients to feel they are being embraced by la familia, whatever their background. Read more about Camino Nuevo. (Paul
... moreCOLONIE — Capital Region providers and agencies who deal directly with the opioid crisis every day have major concerns about the quality and length of local treatment programs for people battling addiction, according to a new Siena College survey.
The survey of more than 600 professionals in the medical, mental health, social service, nonprofit and law enforcement fields found that a majority believe treatment programs aren't working with addicted individuals long enough and blame insurance companies for refusing to cover comprehensive, adequate treatment.
"As bad as the public thinks this epidemic is, stakeholders know it's worse," said Don Levy, director of the Siena College Research Institute.
Eighty-eight percent of the professionals who were surveyed said the epidemic of opioid-related overdose deaths has gotten worse in recent years, and more than half expect it to continue to get worse.
National data support that conclusion. Drug overdose deaths in the U.S. have more than tripled since 1999, climbing steadily over the years and then accelerating around 2012, when it's believed a crackdown on prescription opioids fueled an illicit market for heroin and fentanyl. In 2016, nearly 64,000 Americans died of drug overdoses. Two-thirds were linked to opioids.
A major area of concern centers around treatment. A majority of survey-takers (55 percent) said they believe a person with an opioid addiction needs more than six months of treatment in order to recover successfully.
While the six-month mark is not a "magic number" for everyone, Dr. Melissa Weimer, an addiction medicine specialist at St. Peter's Health Partners, said that milestone is supported by scientific research into the effects on the brain of drug abuse, addiction and withdrawal.
Repeated drug use hijacks the brain's reward center. Imaging and mapping of the brain after drug use stops has shown that it takes about three months for the reward center to start returning to normal and about six months for it to return to baseline.
"The scary thing about opioids is that once you make it through acute withdrawal, unfortunately there's a stage called post-acute withdrawal that can actually last six months to a year — particularly if you're a person who has been using for a very long time," Weimer said.
The symptoms are mild compared to acute withdrawal, she said, but frequently contribute to relapse.
"It is often felt as kind of a low-lying, constant anxiety," said Weimer. "So you have this continual sense of anxiety and irritability. If you undergo a major stress or have underlying anxiety or depression to begin with it can be a strong relapse trigger."
There is medicine to lessen these symptoms, she said. A doctor might prescribe selective serotonin reuptake inhibitors (SSRIs) or non-habit forming clonidine or hydroxyzine.
So why aren't people getting the treatment they need? Or, if they are, why isn't it successful?
The Siena survey revealed some theories. While a majority of local professionals say most treatment programs in the area are "somewhat" effective at getting patients to overcome addiction, 64 percent say treatment just isn't long enough and identified insurance refusing to cover adequate treatment as a major issue locally.
Almost all of those surveyed say insurers should be required to cover treatment beyond the initial detox period, which Weimer said can take three to 14 days depending on how long somebody used opioids and the type of opioid used. The process can be shortened with medications such as buprenorphine, methadone, clonidine or hydroxyzine, she said.
Local health insurers say they follow rules prescribed by the state Office of Alcoholism and Substance Abuse Services when it comes to covering addiction treatment.
Using a tool known as LOCADTR (Level of Care for Alcohol and Drug Treatment Referral), providers and insurers assess a patient's treatment history, medical and psychiatric background, risk factors and social supports to identify which level of care and treatment setting is most appropriate, safe and effective.
"Every health plan is different," said Dr. Kirk Panneton, vice president and regional executive and medical director for BlueShield of Northeastern New York, which offers plans in the Albany area. "But I think there's no question that there's more coverage now, especially given the concerns these past couple years showing this is an epidemic both locally and nationally."
That may be true, advocates say, but there's no doubt that insurers continue to offer inadequate coverage to individuals with mental health and substance abuse issues. Although state and national parity laws require insurers to provide mental health and substance abuse benefits on par with medical and surgical benefits, not everyone complies.
Since 2014, the New York attorney general's office has reached settlements with at least five insurers, including MVP Health Care in Schenectady, after finding they had violated parity laws.
State lawmakers this week passed legislation requiring insurers to submit annual reports to the state Department of Financial Services outlining their compliance with parity laws. The bill still needs the governor's signature.
"These laws have been on the books for decades now, but we're still seeing disparities," said Stephanie Campbell, executive director of Friends of Recovery-New York, a group that advocates for people in recovery from substance abuse.
People seeking mental health and substance abuse treatment have been subjected to higher specialist co-payments, she said, and are more likely to be denied coverage for inpatient treatment under the guise that it's "not medically necessary," she said.
Not everyone needs inpatient services — someone with a steady job, car, friends and family support system, for example, is better suited for outpatient treatment, Weimer said. Those who lack stable housing, income, transportation and social support systems, however, benefit greatly from intensive, inpatient rehabilitation, she said.
If cost of lengthy or intensive treatment programs is the concern among insurers, Campbell suggests they consider the costs of not providing adequate treatment.
"When you can recover and reintegrate into society, you get a job, you pay taxes, your hospitalizations go down, your arrests go down," she said. "The cost-benefit of treating addiction like any other chronic illness is really overwhelming."